“Cultivating psychological safety: Activating humanness in healthcare”, MGMA Insight Article, July, 2020
In the United States, the healthcare environment is experiencing unprecedented change while responding through crises; and yet healthcare leaders continue to search for ways to succeed in creating environments where staff feel engaged and empowered to provide exemplary patient care. An environment where healthcare staff members feel free to speak up, voice their ideas, take risks and experiment is essential.
Psychological safety is a key differentiator in creating environments where individuals and teams learn together and adapt their responses to increase performance.(1) Healthcare leaders are responsible for ensuring psychological safety is infused into and permeates the teams they lead.
A focus area of leadership today is on staff perceptions of the consequences associated with interpersonal risk taking in the professional environment and the effect this risk taking has on performance. In today’s Volatile, Uncertain, Chaotic, Ambiguous (VUCA) healthcare environments, “fear is the enemy of flourishing,”(2) and those healthcare leaders who create space for psychological safety to flourish will benefit. Amy Edmondson, professor at Harvard Business School, defined psychological safety as “a shared belief that the team is safe for interpersonal risk taking.”(3) This definition shifted the concept of psychological safety from an individual focus to a group level construct; the team shares the belief that one will not be punished or humiliated for speaking up with ideas, questions, concerns or mistakes.(4)
LITERATURE AND EVIDENCE
When leaders are intentional about cultivating and practicing psychologically safe behaviors, they are activating humanness in healthcare through themselves and others. In a knowledge-intensive industry such as healthcare, five types of human exchange are prevalent if psychological safety is present:
- Knowledge is readily shared
- Questions are easily asked
- Help is offered and sought as a regular practice
- Errors are readily admitted
- Feedback is constantly solicited and openly received.(5)
Humanness in healthcare is limited or lost if staff members do not feel free to engage in these forms of interaction for fear of being rejected
or marginalized; being seen as incompetent or ignorant; or being labeled as negative, disruptive or creating conflict.
Several studies have been conducted to understand the impact of speaking up in organizations and two key approaches exist: predicting the occurrence of speaking up and focusing on the reluctance to speak up. Findings suggest that the ability for an individual to speak up is mediated by a perceived sense of psychological safety being present.(6) Markus Baer and Michael Frese added to the construct of team psychological safety to include the formal and informal practices that guide and support trustful interactions within a work environment where a climate exists for employees to speak up without fear of rejection or negative consequences.(7) In terms of reluctance to speak up, James R. Detert and Edmondson examined the notion of implicit voice theories, which are taken-for-granted beliefs in which individuals remain silent and withhold ideas, suggestions and concerns because of perceived interpersonal risk or inappropriateness of speaking up within a hierarchical organization.(8) Implicit voice theories operate at a level below the consciousness and are an automatic response to processing stimulus cues and choosing a response perceived as self-protective.
The ability for staff members to speak up is critical to team learning, team effectiveness and organizational performance. Daphna Brueller and Abraham Carmeli studied the impact of high-quality relationships and team performance in 178 service sector teams. High-quality relationships were defined by three capacities:
- Higher emotional carrying capacity (self-disclosure and self-expression)
- Capacity of the relationship to withstand strain
- Degree of connectivity.(9)
The authors confirmed their hypotheses that high-quality relationships between team members and between team members and their manager cultivated high levels of team psychological safety, which, in turn, positively impacted team learning. Team learning was positively associated with team performance.(10) These results underscore the critical role of leader and manager behavior in cultivating psychological safety through deepening emotional connections and displaying openness and flexibility with the teams they lead.
Alexander Newman, Ross Donohue and Nathan Eva conducted a systematic review of the psychological safety literature summarizing key variables and clarifying important practical implications for organizational outcomes. Psychological safety was identified as a multilevel concept occurring at the organization, team and individual levels and is predictive of learning and performance outcomes across all three. Antecedents of psychological safety
at the individual and team levels are centered on “supportive environments,” which include supportive leadership, colleagues and organizational practices. Psychological safety was the moderator between supportive environments and key outcomes such as knowledge sharing, engagement, creativity, innovation and performance.(11)
Psychological safety was found to be especially critical in environments where speaking up prevented errors and improved patient safety. Multidisciplinary teams at Mayo Clinic and other large healthcare organizations rely on psychological safety as a foundation to their success. Teamwork is at the core of Mayo Clinic’s Model of Care and is demonstrated in the integration of multispecialty care and within interdisciplinary partnerships and teams. For Mayo Clinic to accomplish its strategic goals, it requires all staff members, regardless of organizational role or rank, to work together as a trusting and collaborative.
CREATING AN ENVIRONMENT OF SAFETY
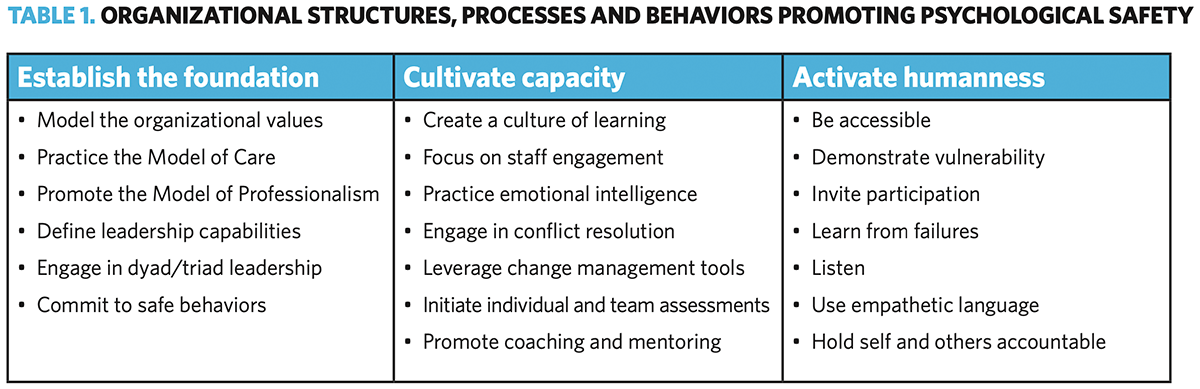
Leaders at Mayo Clinic are charged with creating environments where humanness in healthcare can flourish and demonstrate physical and psychological safety. As an organization with more than 150 years of growth and maturity, Mayo Clinic leaders and staff have designed (and continue to redesign) structures, systems and processes to promote an environment of safety. These structures, systems and processes can be categorized into three overarching strategies (Table 1).
The three strategies depicted in Table 1 contribute to establishing an environment where psychological safety thrives. The tactics listed under each strategy are based on strategies employed by Mayo Clinic and are described in more detail in the following sections.
Establish the foundation. Environments founded on a strong commitment to organizational values, evidence-based models and capabilities offer fertile soil for psychologically safe behaviors to grow and develop. The primary value at Mayo Clinic – “the needs of the patient come first” – is supported by eight core values: respect, integrity, compassion, healing, team-work, innovation, excellence and stewardship. These values are modeled throughout the enterprise, embedded in decision-making and leader and team collaboration, and reinforced using a variety of educational methods and research. The Mayo Model of Care and Model of Professionalism ensure a comprehensive, integrated and compassionate team approach to holistic care. Organizational policies also provide sup- port and further delineate expectations for all team members by defining behaviors.
Effective leadership is a key to organizational success; the Mayo Clinic Leadership Model identifies four foundational capabilities for all leaders to exemplify:
- Inspiring values
- Engaging colleagues
- Bold and forward thinking
- Driving results
Each specialty department has a staff-selected physician chair (or leader) who is partnered with an administrative colleague – together these leaders form the dyad leader partnership.(12) This dyad is responsible for aligning depart- mental initiatives with the organization and cascading the operational plan to the frontline. In the clinical practice arena, the physician
and administrator are joined by a nurse administrator forming a leadership triad. Mayo underscores the highest standards for patient safety, expecting each staff member to follow five safe behaviors in their daily work: pay attention to detail, communicate clearly, have a questioning and receptive attitude, hand off effectively and support each other.
Cultivate capacity. The components in Table 1 offer the foundation for embedding expectations that support an environment of success and safety. There are several ways Mayo Clinic leaders leverage the foundation and take these components to a level deeper by cultivating capacity in their staff. Annually, the organization conducts an enterprise-wide all-staff survey measuring staff satisfaction on key topics related to engagement, culture and overall satisfaction. Leaders practice effective bidirectional communication and co-design customized interventions with individuals and/or their teams. Additional listening strategies such as focus groups, online discussion forums and team and staff meetings provide additional insight into the pulse of the work environment. Annual performance appraisals with 360-degree feedback are an expectation for all employees, including assessment of behavioral performance against the eight core values and individual goal setting for the coming year.
A variety of educational offerings are avail- able for all levels of staff to cultivate a culture of learning. Curricula are designed to build team and individual capacity as well as accelerate readiness for future roles.(13) Content and topical areas include but are not limited to emotional intelligence, effective communication, leading and managing change, effective coaching and mentoring, empowering staff through engagement, leading and managing through crises, creating inclusive environments and developing talent for the future. Individual and team assessments are available upon request with customized interventions in alignment with departmental and organizational strategy.
The structures, systems and processes embedded into daily practice allow for psychological safety to permeate the environment and ultimately impact individual, team and organizational performance.
Activating humanness in healthcare.
While psychological safety is everyone’s responsibility, it is imperative that leadership, from CEO to front-line supervisor, model behaviors that create and sustain a psychologically safe workspace. Leaders have the opportunity to learn from others, to serve and listen, to build trust, to hear and respond to feedback and discover the values of others.(14) Three examples, specific to healthcare, are offered:
- In the operating room, the scrub nurse during the “surgical pause” can raise a question, but it’s how the surgeon responds to that question that creates a safe environment.
- In the laboratory, technicians can ensure their colleagues have a voice in creating a standard operating procedure; but if their supervisor relies only on her favorites and their opinions, other technicians will learn it doesn’t matter what they say.
- In research, a biostatistician may have the support of her colleagues to inform the principal investigator he lacks sufficient data to take his results to the bedside. The investigator can reject the biostatistician’s viewpoint, and, in turn, limit team members from speaking up in the future.
Leaders make it a point to describe the importance of psychological safety in the workplace, explicitly communicating the interdependence each has to the success or failure of an initiative. They explain the rationale behind a decision, the urgency and compelling purpose of a change, and the behaviors needed for collaboration. Leaders create a space for staff to speak up with innovative ideas, and encourage discussion, drawing out the ideas of everyone on the team. In a study conducted at Mayo Clinic, fairness and empowerment were strong predictors of excellence and innovation. More fairness increased psychological safety and trust. More psychological safety and trust increased empowerment, which positively influenced excellence/innovation.(15) The study provides evidence that employees need to feel they are being treated fairly to feel safe in the workplace.
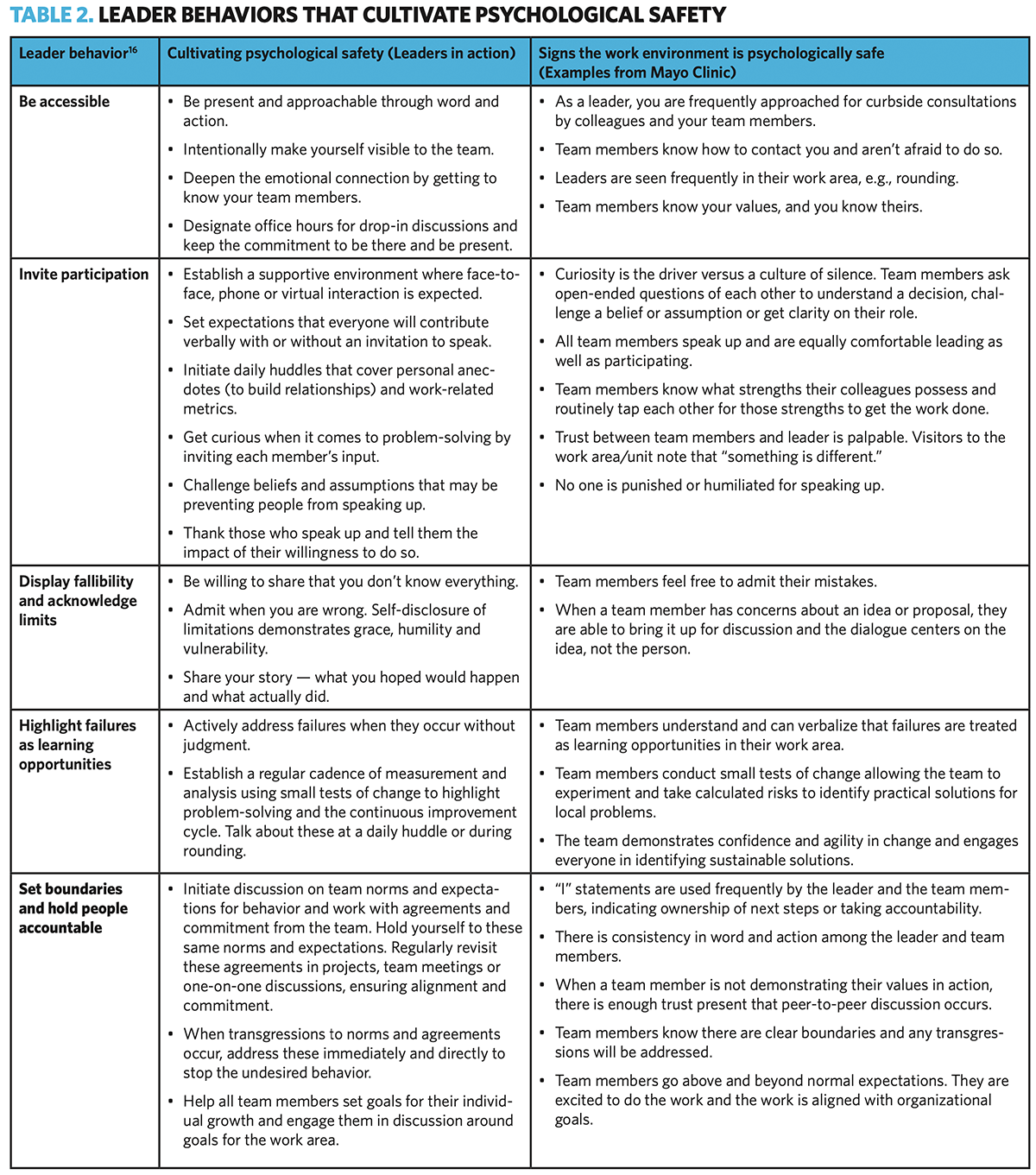
Given the critical role of leaders in setting the stage for psychological safety to take root and grow, Edmondson identifies specific behaviors for every leader to foster (see Table 2, page 45).(16)
Table 2 identifies five leader behaviors, along with the experiences of leaders at Mayo Clinic. Specific behaviors in action are described along with tangible signs that psychological safety is present in the workplace. Frequent acknowledgment of accomplishments and sharing insights gleaned during failures contributes to a safe culture of learning.
CONCLUSIONS
Cultivating psychological safety and activating humanness in healthcare begins with one leader and a commitment to making a difference. One leader can:
- Model inclusion by inviting staff to speak, listening to those comments and acknowledging contributions
- Model their own vulnerability by admitting a mistake, saying they don’t know, asking for help and acknowledging they were wrong
- Model curiosity through the use of open- ended questions, allowing others to consider perspectives different from their own or to voice concerns and challenges.
One leader is enough. Leaders aren’t always in formal, titled roles; they are found throughout the organization; indeed, those who work to create psychologically safe workplaces are leaders. Humanness in healthcare is activated by behaviors that bring to life the structures, systems and processes that ensure psychological safety is present in all facets of the work environment. By cultivating an environment of psychological safety, space is created to hear all voices, all hopes and all fears. Allowing all voices to be heard brings forward self-expression, productive discussions, and, when needed, thoughtful handling of conflict.
NOTES
- Edmondson AC. “Psychological safety and learning behavior in work teams.” Administrative Science Quarterly, 1999, 44(4), 350-383.
- Edmondson AC. The fearless organization: Creating psychological safety in the workplace for learning, innovation, and growth. 2019. Hoboken (N.J.): John Wiley & Sons.
- Edmondson, 1999.
- Edmondson, 2019.
- Edmondson AC. Teaming. How organizations learn, innovate, and compete in the knowledge economy, 2012. San Francisco: Jossey-Bass, Print.
- Edmondson, 1999.
- Baer M, Frese M. “Innovation is not enough: climate for initiative and psychological safety, process innovations and firm performance.” Journal of Organizational Behavior, 2003, 24, 45-68.
- Detert JR, Edmondson AC. “Implicit voice theories: Taken for granted rules of self-censorship at work.” Academy of Management Journal, 2011, 54(3), 461-488.
- Brueller D, Carmeli A. “Linking capacities of high-quality relationships to team learning and performance in service organizations.” Wiley Periodicals Inc, Human Resource Management, July-Aug 2011, 50(4), 455-477.
- Ibid.
- Newman A, Donohue R, Eva N. “Psychological Safety: A systematic review of the literature.” Human Resource Management Review, 2017, 27, 521-535.
- France T, Menaker R, Thielen K. “The importance of radiologist-administrator partnership to future health care.” Journal of the American College of Radiology, 2018, Vol. 16(8), 1,114-1,118.
- Gill P, France T. “Accelerating diverse leader readiness through foresight and futures thinking.” In D. Schreiber and Z. Berge (Eds.), Managing rapid change in technology, globalization and workforce diversity: Using foresight and organizational policy to ensure futures thinking. 327-345. Palgrave Macmillan Publishing.
- Menaker R. “Leadership strategies: Achieving personal and professional success.” Journal of Medical Practice Management, 31 (2016), 336-339.
- Kang JY, Lee MK, Fairchild EM, Caubet SL, Peters DE, Beliles GR, Matti LK. “Relationships Among Organizational Values, Employee Engagement, and Patient Satisfaction in an Academic Medical Center.” Mayo Clinic Proceedings: Innovations, Quality & Outcomes. 2020. 4(1). 8-20.
- Edmondson AC. “The three pillars of a Teaming Culture.” Harvard Business Review. Dec. 12, 2013.